In Australia, face masks for the prevention of disease transmission are considered by the TGA to be a medical device, and therefore must meet TGA Standards to be approved for sale. There are broadly three types recognised by the TGA. Technically, ‘masks’ refers to surgical masks which are the looser, commonly used masks designed for fluid protection, while ‘respirator’ is the correct term for P2/N95 and similar products that provide respiratory protection by filtering inhaled air.
- Surgical Masks (single use surgical or medical) – disposable – fluid resistance and bacterial filtration efficiency. Designed mainly to prevent the emission of larger droplets. Typically blue on the outside, white on the inside. Recommended to be worn for up to 4 hours before disposal. Subdivided into Assigned Protection Factor (APF) of either P1, P2 or P3 – higher is better. Generally widely available.
2. Standard Respirators – single use – disposable – form a tight seal around the face – block microorganisms and submicron airborne particulate materials. Labelled with the efficiency to which they have been tested – e.g.
a. P2 (Australian standard) / N95 (US standard) are very similar apart from slight differences in certification requirements. They both must capture at least 94% of particles in the penetrating size range. Surgical P2/N95 are fluid resistant; Non-surgical P2/N95 are not.
b. The Korean KF94 and Chinese KN95s are similar, though not identical, alternatives.
c. Generally available at pharmacies and hardware stores.
d. Optometrists providing direct patient care to individuals with suspected or confirmed COVID-19, or in zones with a high risk of transmission, should wear P2/N95 standard respirators.
3. Surgical Respirators – single use – as for respirators but are fluid resistant. Intended for performing surgery, aerosol generation of body fluids, or caring for confirmed COVID-19 patients. If a surgical respirator is required but not available, standard P2/N95 respirators can also be used in combination with a surgical mask or face shield to provide fluid resistance.
At least one study, published in the JAMA, has found that respirators with head ties performed better than those with ear loops.
 View
View
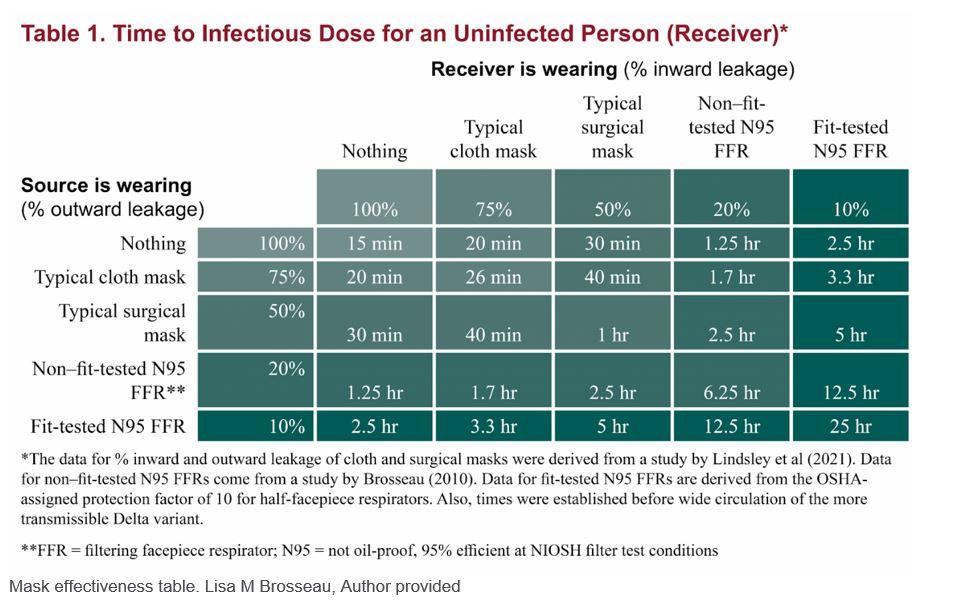 Mask effectiveness table. Lisa M Brosseau, Author provided
Mask effectiveness table. Lisa M Brosseau, Author provided