3:30min
By: Deborah Hackett BMus, LMusA, GradDipHum (It Stud), BA(Hons I), BOptom, MOptom. Optometrist, Victoria. LOOK 2023 scholarship winner.
 Although offered at a growing number of universities in Italy, optometry is not a legislated profession with the scope of practice we have in Australia. Primary eyecare is provided by the ophthalmologist (oculista) in both public and private settings, with the GP also playing a primary care triage role. It is the non-surgical ophthalmologist who most closely corresponds with our role of optometrist.
Although offered at a growing number of universities in Italy, optometry is not a legislated profession with the scope of practice we have in Australia. Primary eyecare is provided by the ophthalmologist (oculista) in both public and private settings, with the GP also playing a primary care triage role. It is the non-surgical ophthalmologist who most closely corresponds with our role of optometrist.
WHY ITALY?
In my pre-optometry days, I had completed a degree in Italian Studies, majoring in Medieval poetry – this was unusual preparation for the optometry course at Melbourne! In 2023, after contemplating my readiness for post-COVID travel, Optometry Australia’s LOOK (Looking Outward on Optometric Knowledge) Scholarship afforded me the opportunity to combine my interests in glaucoma and all things Italian: I took a break from my private practice in Geelong and, reaching out to some old networks, soon found myself scooting around Italy, exploring how the Italians manage glaucoma and its various and changing treatment options.
Congresso Nazionale Società Italiana del Glaucoma (S.I.GLA) – Centro Lingotto, Turin (15-17 June)
This was the first conference I attended and an add-on to my original proposal. Hosted in Turin, the original capital of Italy at its unification in 1861, the conference was held in the old FIAT factory, now converted into a shopping mall and conference centre. The original 1.5km rooftop test track remains largely as it was when it featured in the iconic chase scene of the 1969 movie, The Italian Job, and served as a novel location (with the exit clearly marked) for the al fresco conference dinner and pre-dinner passeggiata!
After a quick peek in the National Museum of Cinema, where I stumbled across a series of rooms with interactive displays on optics and the camera oscura, I was drawn into a 3-day whirlwind of Italian camaraderie, back-to-back lectures, live surgery feeds and stimulating lunchtime debates.
Italians are key collaborators within the European Glaucoma Society and are keen contributors to the international body of research and literature on glaucoma. Of most recent impact on the current shift in glaucoma management has been SIGLA president, Stefano Gandolfi’s retrospective study on annual delivery of low intensity Selective Laser Trabeculoplasty (SLT) at the University Hospital in Parma (2018)[i]. This was then expanded upon by the United Kingdom/United States team, led by Tony Realini and Gus Guzzard, to form the multicentre COAST trial[ii] which is currently actively recruiting participants.
World Glaucoma Congress (WGC) – La Nuvola, Rome (28 June – 1 July)
The 10th Anniversary WGC was held at La Nuvola Convention Centre, a modern eco-friendly structure located in the 1930s abandoned Fascist precinct of EUR, Rome. Standout speakers were Ike Ahmed (Canada) and Paul Singh (USA), industry leaders in Minimally Invasive Glaucoma Surgery (MIGS) and whose research outputs include the COMPASS[iii], HORIZON[iv] and STAR-GLOBAL[v] trials.
 Ahmed and Singh are both champions of Interventional Glaucoma (IG) – a proactive mindset approach focussing on early diagnostics with advanced monitoring systems that support safe, non-destructive intervention early in the disease process. This proactive approach to early intervention has been largely facilitated by developments in alternative laser technologies (excimer, femtosecond and Nd:YAG) which have led to minimally and non-invasive, non-incisional and non-contact procedures to lower and maintain intraocular pressure (IOP) targets. IG marks a shift away from topical glaucoma medications due to emerging data on long term morphological changes of the ocular surface and failure to maintain a steady IOP. In the longer term, the ongoing use of topical therapies can have a negative impact on surgical outcomes that are also more likely to be required if IOP cannot be successfully maintained. The overarching goal of IG is improved patient quality of life, both disease and treatment related.
Ahmed and Singh are both champions of Interventional Glaucoma (IG) – a proactive mindset approach focussing on early diagnostics with advanced monitoring systems that support safe, non-destructive intervention early in the disease process. This proactive approach to early intervention has been largely facilitated by developments in alternative laser technologies (excimer, femtosecond and Nd:YAG) which have led to minimally and non-invasive, non-incisional and non-contact procedures to lower and maintain intraocular pressure (IOP) targets. IG marks a shift away from topical glaucoma medications due to emerging data on long term morphological changes of the ocular surface and failure to maintain a steady IOP. In the longer term, the ongoing use of topical therapies can have a negative impact on surgical outcomes that are also more likely to be required if IOP cannot be successfully maintained. The overarching goal of IG is improved patient quality of life, both disease and treatment related.
HOSPITAL AND CLINIC VISITS

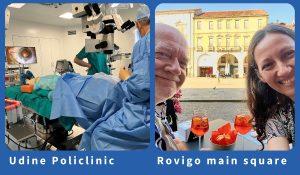
Between the two conferences I whipped around northern and central Italy observing surgery and participating in consultations at hospitals, polyclinics and private practices. I was also taken to visit a beautiful 3 storey Centro Ottico (pictured right) complete with laboratory, warehouse, consulting rooms and a museum – a family business for 5 generations!
For those I was unable to catch at their workplace, a home cooked meal or an Aperol Spritz in the piazza afforded an enviable setting for cultural exchange and discussions on healthcare, business models, politics, and glaucoma management. One of my most memorable days was a walk in the Italian Alps with a glaucoma surgeon and his emergency surgeon hiking buddy. Over discussions on ab interno versus ab esterno MIGS, the pros and cons of a deep sclerectomy and appendectomy umbilical port sites, we found ourselves surrounded by cows… and in Austria!
OBSERVATIONS AND INSIGHT
Throughout the conferences and clinical visits in Italy, I constantly witnessed a high level of care and attention to detail, involvement and enthusiasm in contributing to an international dialogue of research and collaboration, and practitioners who were always striving for the best patient outcomes. However, in the absence of a primary/secondary eyecare system, the public hospital resources seemed unnecessarily tied up with conditions such as blepharitis and amblyopia. The surgeons tending to these patients had skills and expertise far beyond what was often required. This highlighted to me the importance of optometry in the division of labour and in providing an inherent triage where conditions such as Normal Tension Glaucoma are less likely to fall through the cracks.
I graduated in the wake of the Ocular Hypertension Treatment Study (OHTS)[vi] with the clear message that not every ocular hypertensive would progress to glaucoma. We were encouraged to not overtreat, but to take good baselines and be ready to initiate treatment if change over time was determined. Ahmed’s favourite expression that “glaucoma is only young once” reflects the pendulum swinging back. Early-stage glaucoma (and at risk OHT) is the one opportunity we have to change the course of the disease by intervening early and hard. The difference now is that technological advancement, within a growing body of research, has facilitated more honed and controllable treatments, making that intervention less invasive, lower risk and thus safer for the patient in the longer term.
First line Selective Laser Trabeculoplasty (SLT)
The main outcome of these latest developments in glaucoma management, driven largely by the studies in the landmark LiGHT trial[vii],[viii], is that SLT is now widely accepted as first line treatment in glaucoma and OHT. The European Glaucoma Society and the American Academy of Ophthalmology have recently updated their glaucoma management guidelines to recognize or recommend SLT as an initial intervention for glaucoma and OHT.
The United Kingdom was the pioneer, however, conducting an exceptional surveillance review[ix] Of the NICE guidelines on glaucoma management in 2019 in direct response to the 3-year LiGHT publication. This emergency intervention panel instructed an immediate update of their guidelines – that SLT be offered as first-line treatment BEFORE drops in glaucoma and OHT.
The Italians are already putting this into practice, but what about Australia?
As of yet, we still lack any formalised change of process. The NHMRC glaucoma guidelines (2010) are becoming ragged and, for optometrists, largely superseded by Optometry Australia’s Clinical Practice Guide for the Diagnosis and Management of Open Angle Glaucoma 2020 (due for revision in 2024). Whilst the Brits were laser quick (sorry) in their response to the 3-year LiGHT trial, the Optometry Australia guidelines acknowledge that “SLT is being considered first-line therapy in some cases”, but the overriding emphasis of this document is on topical pharmacotherapy.
Australia, no doubt, will eventually follow suit, and when it does, the higher demand on ophthalmology for SLT may not be easily met. As optometrists are proficient in biomicroscopy, SLT should fall naturally under our skill set.
Optometrists performing advanced procedures is not a novel idea. We are behind the United Kingdom, United States and New Zealand where in certain regions and settings (in conjunction with ophthalmologists) optometrists can already perform anterior laser procedures, such as Nd:YAG capsulotomy and SLT. Back in Australia we are still lobbying for oral medication prescribing rights.
Singh acknowledges that gonioscopy may be a deterrent for practitioners embracing SLT in general, as it can be challenging and awkward for both practitioner and patient. The Belkin Direct Selective Laser Trabeculoplasty (DSLT) and ViaLase FLigHT harness the latest developments in laser technology, making the procedure more comfortable and safe, overcoming some of the challenges associated with traditional SLT. This may be another avenue for SLT-type procedures to become more accessible to optometry.
Yet there are still many obstacles to negotiate: legislation, training, equipment cost or access, mindset, and support from ophthalmology. The non-surgical ophthalmologists in Italy, some of whom have been surgeons, offered a lot of insight into managing post-procedural complications and follow-up.
If optometrists can be recruited to administer COVID vaccinations in time of need, is SLT such a far cry when we can already use a slit lamp and a gonio prism? If our system could better utilise the resources in optometry, could we not alleviate the 5-year waitlist for cataract surgery in Geelong?
Before heading home, I detoured to Wales where I took refuge from the heat, ate an early dinner, and reflected on my overwhelmingly jam-packed time in Italy. It was such a valuable experience being amidst the buzz of industry professionals, researchers and surgeons, becoming excited about new research, techniques and equipment and even meeting some fellow Australians! The stimulation of learning and debating in another language refreshes me to come home to the daily grind with new enthusiasm.
Returning to Melbourne my luggage took a 5-day deviation to Los Angeles with a few of my essential items, and I found that my post-COVID travel itch had been scratched for now.
About Optometry Australia’s LOOK Scholarships
Launched in 2020, the LOOK International program was established to evolve optometric scope of practice by funding member-led study tours that investigate international optometric advancements that are not yet available, or readily available, in Australia. Scholarships for 2025 will be launched in late 2024. Contact policy@optometry.org.au to find out more.
[i] Gandolfi SA, Ungaro N, Varano l, Saccà S. Low Power Selective Laser Trabeculoplasty (SLT) repeated yearly as primary treatment in Open Angle Glaucoma(s): Long term comparison with conventional SLT and ALT. Investigative Ophthalmology & Visual Science. 2018;59(9):3459-.
[ii] Realini T, Gazzard G, Latina M, Kass M. Low-energy Selective Laser Trabeculoplasty Repeated Annually: Rationale for the COAST Trial. Journal of glaucoma. 2021;30(7):545-51.
[iii] Vold S, Ahmed, II, Craven ER, Mattox C, Stamper R, Packer M, et al. Two-Year COMPASS Trial Results: Supraciliary Microstenting with Phacoemulsification in Patients with Open-Angle Glaucoma and Cataracts. Ophthalmology. 2016;123(10):2103-12.
[iv] Ahmed IIK, Rhee DJ, Jones J, Singh IP, Radcliffe N, Gazzard G, et al. Three-Year Findings of the HORIZON Trial: A Schlemm Canal Microstent for Pressure Reduction in Primary Open-Angle Glaucoma and Cataract. Ophthalmology. 2021;128(6):857-65.
[v] Denis P, Hirneiß C, Durr G, Reddy K, Kamarthy A, Calvo E, et al. Two-year outcomes of the MINIject drainage system for uncontrolled glaucoma from the STAR-I first-in-human trial. The British journal of ophthalmology. 2020;106.
[vi] Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA, et al. The Ocular Hypertension Treatment Study: Baseline Factors That Predict the Onset of Primary Open-Angle Glaucoma. Archives of Ophthalmology. 2002;120(6):714-20.
[vii] Gazzard G, Konstantakopoulou E, Garway-Heath D, Garg A, Vickerstaff V, Hunter R, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. The Lancet. 2019;393(10180):1505-16.
[viii] Gazzard G, Konstantakopoulou E, Garway-Heath D, Adeleke M, Vickerstaff V, Ambler G, et al. Laser in Glaucoma and Ocular Hypertension (LiGHT) Trial: Six-Year Results of Primary Selective Laser Trabeculoplasty versus Eye Drops for the Treatment of Glaucoma and Ocular Hypertension. Ophthalmology. 2023;130(2):139-51.
[ix] 2019 exceptional surveillance of glaucoma: diagnosis and management (NICE guideline NG81). London: National Institute for Health and Care Excellence (NICE); 2019.
Tagged as: Awards - honours - grants, Glaucoma, member profile