1:30min
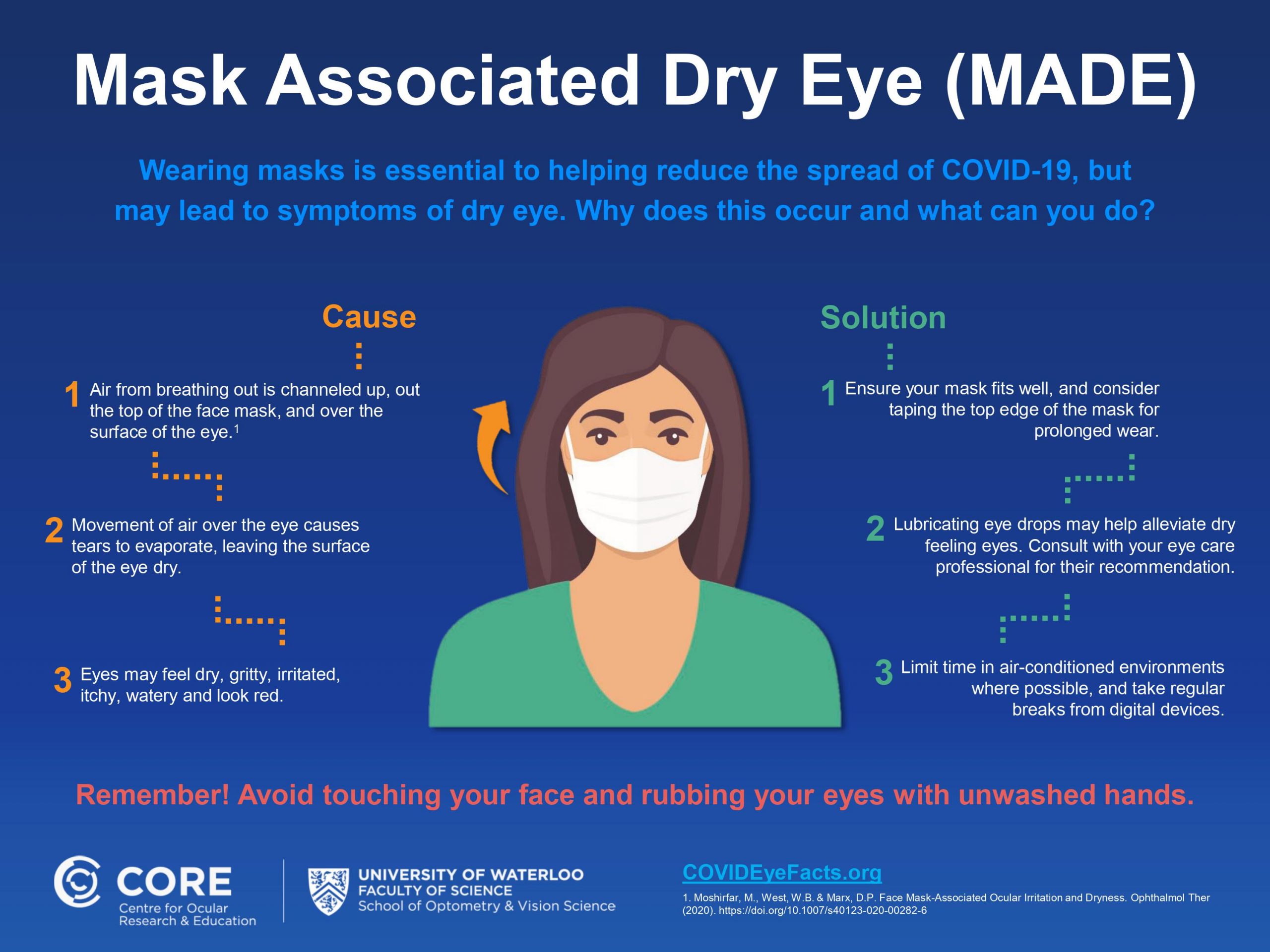
Image, Centre for Ocular Research and Education
By Helen Carter
Journalist
Optometrists are being advised to look out for increased cases of dry eye after Canadian researchers named and reported a new phenomenon – mask-associated dry eye or MADE – due to the widespread use of face masks to combat COVID-19’s spread.
Experts from the Centre for Ocular Research & Education (CORE) at the University of Waterloo’s School of Optometry and Vision Science said there had recently been increased reports of dry eye and a recent review from American researchers concluded that eye dryness and irritation from mask wear may become a problem for a large percentage of the population.
Director of CORE, optometrist Professor Lyndon Jones, advised eye care professionals how to recognise mask-associated dry eye and methods to mitigate the condition.
‘Face masks are crucial in the fight against COVID-19 and eye care professionals are well-positioned to provide patients with advice on appropriate wear in order to maximize eye comfort,’ he said. ‘Asking patients about their mask-wearing experiences and providing a few helpful tips takes little time and can make a substantial difference.
‘Masks significantly reduce the outward spread of air. However, exhaled air still needs to disperse and when a mask sits loosely against the face the likely route is upwards. This forces a stream of air over the surface of the eye, creating conditions that accelerate tear film evaporation, leading to dry spots on the ocular surface and discomfort.
‘As well as worsening symptoms in patients with pre-existing dry eye disease, MADE can affect the elderly who typically have a poorer quality tear film, contact lens wearers, and masked people working extended hours in air-conditioned settings and/or while using digital screens.’
MADE may also encourage people to rub their eyes for temporary relief—raising the possibility of unwashed hands being brought to the face which, in turn, increases the likelihood of coronavirus infection through the mouth, nose, and to a lesser extent, the eye, he said.
Guidance for optometrists
CORE suggests that optometrists consider incorporating three MADE-related actions into their examination protocols:
- Consider the role of the face mask if there are worsening symptoms and signs in patients with confirmed dry eye disease, or if patients report dry, uncomfortable eyes or variable vision for the first time.
- Routinely ask all patients how their eyes feel while wearing a mask, since many may not think to volunteer their experiences or associate their symptoms with mask use.
- Provide advice on alleviating symptoms, including using the CORE-developed infographic (above) to show how a few simple steps can likely provide relief and minimise reoccurrence.
Tips for patients
CORE recommends that mask wearers experiencing dry eye symptoms try straight-forward solutions:
- Ensure that a mask is worn appropriately, particularly with spectacles or sunglasses. A carefully taped top edge that does not interfere with blinking may help.
- Apply lubricating drops, asking their optometrist for recommendations.
- Limit time in air-conditioned environments and take regular breaks from digital devices.
Professor Jones, a popular speaker at many Optometry Australia state conferences over recent years, stressed that people should first check with their optometrist for advice and to rule out other causes of dry eye. He was also adamant that bringing attention to MADE should not be used to support anti-mask wearing sentiments.
‘Responsibly wearing a mask, even when having to contend with eye dryness, is a critical part of overcoming the global pandemic,’ he said.
‘The good news is that we understand MADE and can address it. It is an opportunity for eye care professionals to further communicate their knowledge and ongoing value to patients at a time when sound, scientific guidance is needed more than ever.’
American researchers from the Department of Ophthalmology and Visual Sciences, John A. Moran Eye Center, University of Utah said in Ophthalmology and Therapy that they had observed an increase in ocular irritation and dryness among regular mask users. They also said irritation of the ocular surface associated with mask use raised concerns for increased risk of disease transmission through the ocular route.
‘In our community and patient population, we have seen a marked increase in dry eye symptoms among regular mask users at multiple local clinics,’ they wrote.
‘This group includes individuals who have never previously suffered from dry eyes. Individuals using masks regularly for an extended duration appear more likely to show symptoms. This group includes the elderly, immuno-compromised, and clinic staff who wear masks almost full-time.’
Staff members using taped masks to prevent air convection toward the eyes also complained of corneal irritation and in these cases, researchers postulated that the tape adhering to the skin of the upper cheek may interfere with the normal excursion of the lower eyelid, possibly inducing mechanical ectropion with secondary lagophthalmos.
‘Masks with a pliable nose-wire should be used, with attention toward fitting the shape of the wire to prevent air being directed toward the eyes,’ they wrote. ‘Masks can also be taped at the top to impede upward airflow, but care should be taken to ensure that lower lid excursion is not inhibited.’
FDA approved cabeau tape pre-cut mask securing strips are a new option to seal gaps around masks and prevent glasses fogging.
Read also, How to stop your glasses fogging when wearing a face mask on our Good Vision for Life website.
Tagged as: COVID-19, Dry eye, International, Patient management, Universities