1:30min
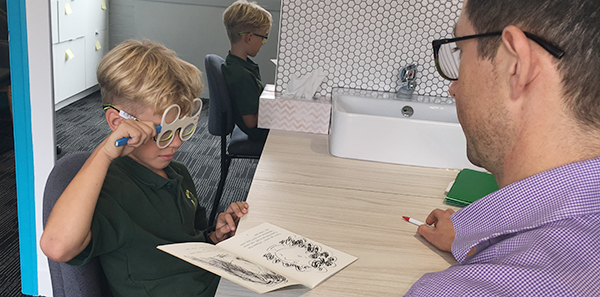
Peter Nixon with a patient, not Ethan
______________________________
By Peter Nixon
Behavioural optometrist
The simplest of optometric cases can have some underlying vision dysfunctions that may lead to large problems.
Ethan, an eight-year-old male Caucasian, presented complaining of having had constant blur in the distance for at least 18 months. He noted that before this time he had had transient blur in the distance after reading. He now had to sit close to the board to see what his teacher had written and he often squinted.
Ethan was a prolific reader who loved school and was an enthusiastic piano player. He was noted to be a high achiever and often became frustrated if things didn’t go to plan. He would often skip words when reading and tended to pull his print closer where things looked and felt better. He had no notable health problems but family history showed myopia and astigmatism on his maternal side.
Clinical examination revealed Ethan to have reduced acuities of R 6/30 L 6/38. Retinoscopy found that he was shortsighted. Careful refraction and binocular blur function revealed R -1.50 DS L -1.75 DS (max plus to 6/6). Further examination with his new script in place revealed that his eye tracking skills were still developing and he had accommodation insufficiency with a large lag of accommodation (+1.5 OU).
Techniques such as the Brock string, cover test and the Howell phoria card also revealed a large esophoric posture (lead) at near. This increased with more accommodative demand and time. His stereo contour acuity was reduced with the Wirt contour circles (50 seconds of arc).
Ethan and his family were offered options for optical correction, including multifocals, low dose atropine and orthokeratology. They opted for a pair of multifocal glasses to correct his myopia, with a +1.50 Add, which has been shown to have some effect on slowing progression in myopic individuals with esophoria and relieve accommodative asthenopia and tonic accommodation.1,2
Orthokeratology was strongly recommended for the future as this has been shown to consistently achieve a decrease in progression3,4 by reducing peripheral retinal blur.5,6
Ethan was recommended to use visual hygiene, which included holding his print further away, working only one hour at near before taking breaks when he was to go outside to play,7 using good lighting and looking away from his work from time to time into the distance.
He and his parents also agreed to undertake vision therapy to improve eye movements, his accommodation system and divergence skills. This also focused on peripheral awareness as myopes and esophoric patients tend to be very centrally-focused people.
Ethan’s vision therapy started initially with monocular accommodative work with low powers and was quickly enhanced through bi-ocular and binocular work. In all of the techniques the aim was to achieve quick focus and alignment.
At review, Ethan had adopted a more distant reading posture at near, was not skipping lines or words when reading and was doing better with comprehension at school. His tracking and reading eye movements were controlled and his stereo had improved (40 seconds of arc on the Wirt circles and 20 seconds of arc on the Randot circles).
He now achieved an ortho posture on the Howell phoria card without his Add and slight exophoria with it. He was more comfortable in his visual environment.
Integrating vision therapy into Ethan’s treatment plan had created an environment where he was more willing to work and had encouraged a better posture that may also slow his myopia progression, along with good visual hygiene.
NOTE: The patient’s name has been changed to ensure privacy
1. Leung JT, Brown B. Progression of myopia in Hong Kong Chinese schoolchildren is slowed by wearing progressive lenses. Optom Vis Sci 1999; 76: 346–354.
2. Gwiazda JE, Hyman L, Norton TT, Hussein ME et al. Accommodation and related risk factors associated with myopia progression and their interaction with treatment in COMET children. Invest Ophthalmol Vis Sci 2004; 45: 2143–2151.
3. Downie L et al. Corneal Reshaping Influences Myopic Prescription Stability (CRIMPS): An analysis of the effect of orthokeratology on childhood myopic refractive stability eye & contact lens. Science Clinical Practice 2013; 3: 4: 303-310.
4. Swarbrick HA, Alharbi A, Watt K et al. Myopia control during orthokeratology lens wear in children using a novel study design. Ophthalmology 2015; 122: 620–630.
5. Atchison DA, Pritchard N, Schmid KL, Scott DH et al. Shape of the retinal surface in emmetropia and myopia. Invest Ophthalmol Vis Sci 2005; 46: 2698–2707.
6. Atchison DE, Li S-M et al. Relative peripheral hyperopia does not predict development and progression of myopia in children. Invest Ophthalmol Vis Sci 2015; 56: 10: 6162-6170. doi: 10.1167/iovs.15-17200.
7. Dirani M, Tong L, Gazzard G, Zhang X et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol 2009; 93: 997-1000.
Also
Gwiazda et al. A dynamic relationship between myopia and blur-driven accommodation in school-aged children. Vision Research 1995; 35: 1299–1304.