1:30min
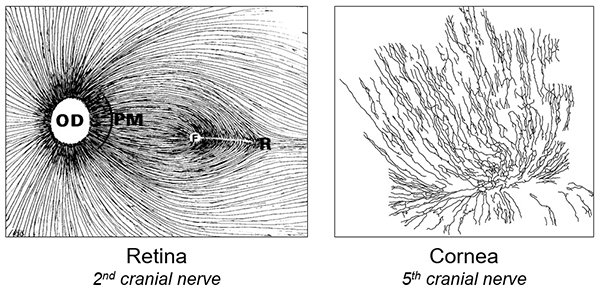
Deficits in the structure and function of the rich nerve plexus in the cornea and retina can indicate the presence of diabetic neuropathy. Image, Professor Nathan Efron.
______________________________
By Helen Carter
Journalist
Optometrists can help prevent diabetic foot amputations by using their OCT to detect early nerve damage in limbs and alert doctors and patients, optometrist Professor Nathan Efron says.
Professor Efron will speak about expanding the role of optometry in diabetes management and ophthalmic assessment of diabetic neuropathy at Optometry Western Australia’s WAVE congress from March 30-31.
‘The leading cause of amputations is foot ulcers from diabetic neuropathy but optometrists can help prevent this by detecting early signs of diabetic neuropathy when looking at patient’s eyes,’ he told Optometry Australia. ‘The main role optometrists have in diabetes patients is to screen for diabetic retinopathy but they can extend their scope of practice to detect diabetic nerve damage to limbs.’
Every day 12 Australians undergo a diabetes-related amputation, with more than 4,400 mostly preventable amputations occurring annually, and 10,000 hospital admissions a year for diabetes-related foot ulcers, according to Diabetes Australia.
Professor Efron, Professor Emeritus of Queensland University of Technology’s School of Optometry and Vision Science, and editor of Optometry Australia’s journal, Clinical and Experimental Optometry, also has first-hand experience as a person with diabetes.
‘About 50 per cent of diabetes patients experience diabetic peripheral neuropathy (DPN) at some level with symptoms including numbness, tingling or pain in the arms and legs,’ he said. ‘One of the main complications is losing nerve sensation in the feet and patients with numbness may be unaware of foot trauma which can develop into an ulcer and may require amputation.’
Image, Diabetes Australia
For 10 years Professor Efron has been using corneal confocal microscopy, equipment mainly used in research laboratories, to study nerve fibres in the corneas of patients with diabetic neuropathy.
Fewer nerves in cornea
‘People with diabetic neuropathy have fewer nerves in the cornea,’ he said. ‘A two-minute examination will show this and in future this could be a screening test for diabetic peripheral neuropathy.
‘Optometrists already use optical coherence tomography (OCT) to examine the retina in people with diabetes, and are able to detect retinal nerve fibre layer thinning. Thinning of the retinal nerve fibre layer is a signal that the person could have peripheral diabetic neuropathy in other sites.
‘Our research shows that retinal nerve fibre thinning is a very early marker of loss of fine nerve fibres around the body occurring at the same time as in the eye. This could lead to more overt loss of sensation in the feet.’
Professor Efron said optometrists could record this observation in their patient notes and also mention it along with the possibility of DPN when writing letters to doctors about their diabetes patients.
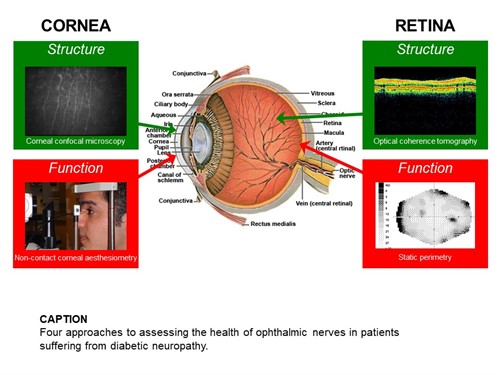
Four approaches to assessing the health of ophthalmic nerves in patients suffering from diabetic neuropathy. Image, Professor Nathan Efron.
Optometrists are expected to deliver thousands of extra comprehensive eye examinations to diabetes patients through the new national KeepSight program so will be seeing more diabetes patients.
‘If retinal nerve fibre layer thinning is severe, immediate referral to a doctor may be required to further investigate for DPN but if mild or moderate, record this in patient notes and notify their GP,’ he said.
‘Even if optometrist do not have an OCT, it’s simple to ask all diabetes patients if they are experiencing any loss of sensation or tingling in the arms or legs.
‘Research findings from our LANDMark study have been published widely and some optometrists are already doing this but I am talking at conferences like WAVE to get the message out that we have technology in our practices we can use and be alert to detecting early stage diabetic neuropathy.
In sync with Optometry 2040
‘Expanding the role of optometry in diabetes management is in sync with Optometry Australia’s policy document Optometry 2040, which looks at what clinical optometry might look like in 2040.
‘These sorts of advanced techniques for the early detection of diabetic neuropathy may well be a key aspect of optometric practice in the future, and may include monitoring progression of DPN and effects of interventions.’
Findings from the Longitudinal Assessment of Neuropathy in Diabetes using novel ophthalmic MARKers (LANDMark) study have been reported in more than 70 publications. The study is ongoing, due to the National Institutes of Health extending funding for its researchers to join with five laboratories globally in an extended multi-centre study of about 1,000 patients, with more in the pipeline.

The LANDMark team, led by study director Professor Nathan Efron, front centre. LANDMark is an acronym for Longitudinal Assessment of Neuropathy in Diabetes using novel ophthalmic MARKers
Professor Efron said, when publishing initial findings in Optometry and Vision Science: ‘With further validation, these ophthalmic markers could become established as rapid, painless, non-invasive, sensitive, reiterative, cost-effective and clinically accessible means of screening for early detection, diagnosis, staging severity and monitoring progression of DPN and assessing effectiveness of possible therapeutic interventions.’
He said the corneal epithelium of diabetic patients was more fragile, corneal sensitivity was reduced and patients may be unaware or less aware of corneal trauma or infection. Recovery from corneal trauma in diabetic patients with neuropathy may be worse than for diabetic patients without neuropathy. For this reason, those with severe DPN should exercise extreme caution if wearing contact lenses.
Visual dysfunction in patients with DPN plus impaired mobility and slower rates of tissue healing in the limbs following injury could increase falls risk.
Optometrists screening for and assessing DPN should anticipate the possibility of observing changes in diabetic patients with neuropathy including reduced corneal nerve fibre density, corneal
sensitivity loss, RNFL thinning and loss of peripheral visual field sensitivity, he said.
Other features at WAVE:
WAVE19 at Fremantle Esplanade Hotel, offers up to 40.5 CPD points, including 21 therapeutic points. Saturday morning clinical workshops run concurrently and repeat four times while lectures feature on Saturday afternoon and Sunday.
On Sunday morning there will be separate ECO CPD lectures for early career optometrists (ECOs), and a dispensers session. ECOs who attend the Sunday morning session and want to join Sunday afternoon or Saturday sessions qualify for discounted registration.
There will also be a sundowner on Saturday evening.
Tagged as: Diabetes, Patient management