1:30min

By Helen Carter
Journalist
More Indigenous Australians are accessing eye health services than ever before, with nearly one in three using eye health services, and one in seven having eye examinations by an optometrist or ophthalmologist, a new report reveals.
Optometrists are playing a major part in the improvement, including through the Visiting Optometrists Scheme as the number of services provided through VOS in mainly regional and remote areas more than tripled from 8,298 occasions of service between 2010–2011 to 25,849 in 2018–2019.
The Australian Institute of Health and Welfare Indigenous eye health measures 2020 report was launched virtually today by the Minister for Health, the Hon Greg Hunt MP.
The report revealed that in the past decade or so, the proportion of Indigenous Australians who had had an eye health check increased from 11 per cent to 30 per cent, and 13 per cent of Indigenous Australians (about 100,700) had an eye examination by an optometrist or ophthalmologist in 2018–2019, based on MBS claims.
Rates of screening for diabetic retinopathy and cataract surgery also rose in this population, while trachoma rates fell more than threefold in young Indigenous children.
Despite the good news, the report’s authors warned that many Aboriginal and Torres Strait Islander people still face barriers in accessing eye health services including financial, cultural, social and locational barriers.
‘If barriers to accessing eye health services can be overcome, most of the blindness and vision impairment experienced by Indigenous Australians could be prevented or treated, particularly vision loss due to refractive error, cataract and diabetic retinopathy,’ the report states. ‘For example, use of glasses and cataract surgery are two relatively low-cost, effective interventions for treating the main causes of vision loss.’
The report provides an evidence base for monitoring changes in Indigenous eye health over time, access to and use of eye health services, and for identifying gaps in service delivery. The 23 Indigenous eye health measures cover the prevalence of eye health conditions, diagnosis and treatment services, the eye health workforce and outreach services.
Source: Australian Institute of Health and Welfare
Highlights from the fourth annual report on Indigenous eye health measures reveal the following statistics about Indigenous Australians:
- The proportion who had an eye health check as part of a health assessment increased between 2010–2011 and 2018–2019 from 11 per cent to 30 per cent (based on age-standardised rates.)
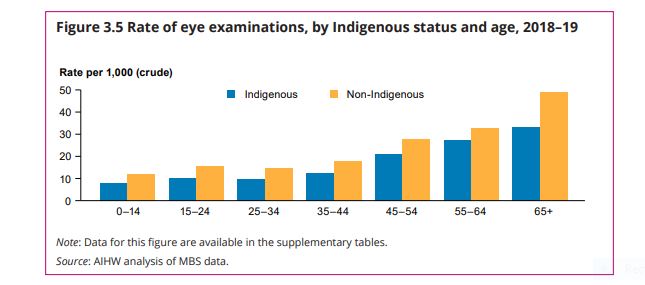
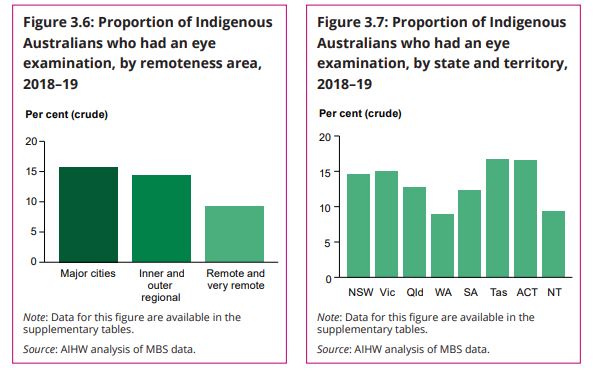
- In 2018–2019, 13 per cent (about 100,700) had an eye examination by an optometrist or ophthalmologist. The age-standardised proportion of Indigenous Australians who had an eye examination jumped from 14 per cent in 2008–2009 to 16 per cent in 2018–2019 compared with a rise from 17 per cent to 22 per cent for non-Indigenous Australians. Rates of eye examinations for Indigenous Australians were highest in Tasmania and the ACT and lowest in WA.
- The number of services provided under the Visiting Optometrists Scheme have fluctuated, but overall services more than tripled from 8,300 to 25,850 between 2018–2019 and 2010–2011. The highest number of occasions of service were provided in country WA and the NT while the highest rates of service were in country WA and Western Queensland.
- The age-standardised cataract surgery rate rose 42 per cent to about 7,400 hospitalisations per 1,000,000 population from 2008–2010 to 2016–2018.
- In 2018–2019, 16,780 spectacles (26 per 1,000 population) were dispensed under state spectacle schemes by New South Wales, Victoria, Queensland, South Australia and Tasmania (states and territories able to provide data). Of these, Victoria (2,589 spectacles, 42 per 1,000 population) came closest to meeting the estimated number of spectacles needed—66 per cent of the population-based need met.
- Among those who had a diabetes test, the age-standardised proportion who were screened for diabetic retinopathy rose from an estimated 31 per cent in 2008–09 to 37 per cent in 2018–19.
- The estimated prevalence of active trachoma among children aged five to nine in at-risk communities fell from 15 per cent in 2009 to 4.8 per cent in 2012 and has since plateaued around this level (4.5 per cent in 2019.)
- In 2019, the overall treatment coverage of active trachoma cases in at-risk communities was 89 per cent, meaning 4,711 of 5,294 community members identified as requiring treatment received antibiotics including children with active trachoma, their household contacts and other community members.
- In 2018 fewer than 10 optometrists identified as Indigenous Australians.
- Indigenous Australians over the age of 40 have nearly three times the rate of vision loss of other Australians (Foreman et al. 2016) but there is some evidence of improvement, with findings of the 2016 National Eye Health Survey indicating that the prevalence of blindness among Indigenous Australian adults has declined, possibly related to improvements in prevention and treatment services.
- The main causes of vision loss for Indigenous Australians aged 40 and over are refractive error (61%), cataract (20%) and diabetic retinopathy (5.2%) compared with refractive error (61%), cataract (13%) and age-related macular degeneration (10%) for other Australians aged 50 and over. (2016 National Eye Health Survey.)
Source: Australian Institute of Health and Welfare
The Australian Government has committed to ending avoidable blindness in Indigenous communities by 2025 and is funding a range of initiatives to prevent and treat vision loss including a new National Agreement on Closing the Gap.
Optometry Australia’s National Policy Manager, Skye Cappuccio, an advisory group member for the report, said: ‘The report highlights some of the progress that has been made, particularly in terms of Aboriginal and Torres Strait Islander people’s access to eye care services.
‘The expansion of the Visiting Optometrists Scheme (VOS) has been one important element in this, and the optometrists involved in providing these important outreach services should be acknowledged for the important role they play. While there have been notable and welcome increases in Commonwealth funding for the VOS over the last decade, further investment still is needed to ensure access to culturally safe primary eye care.’
Ahpra’s inaugural Aboriginal and Torres Strait Islander Employment Strategy
The report was launched on the eve of NAIDOC Week, November 8 to 15, 2020, NAIDOC (National Aborigines and Islanders Day Observance Committee) Week celebrations across Australia each year celebrate the history, culture and achievements of Aboriginal and Torres Strait Islander Peoples.
On Monday, Ahpra CEO Martin Fletcher will launch Ahpra’s inaugural Aboriginal & Torres Strait Islander Employment Strategy 2020 – 2025, a key deliverable for the National Scheme’s Aboriginal and Torres Strait Islander Health and Cultural Safety Strategy 2020–2025.
The goal of the Employment Strategy is to increase Aboriginal and Torres Strait Islander participation within Ahpra through the development of a culturally safe work environment that reflects the diversity of the communities in which we operate and serve.
Tagged as: Eye examinations, Indigenous eye health, Patient management, Remote & rural optometry