1:30min
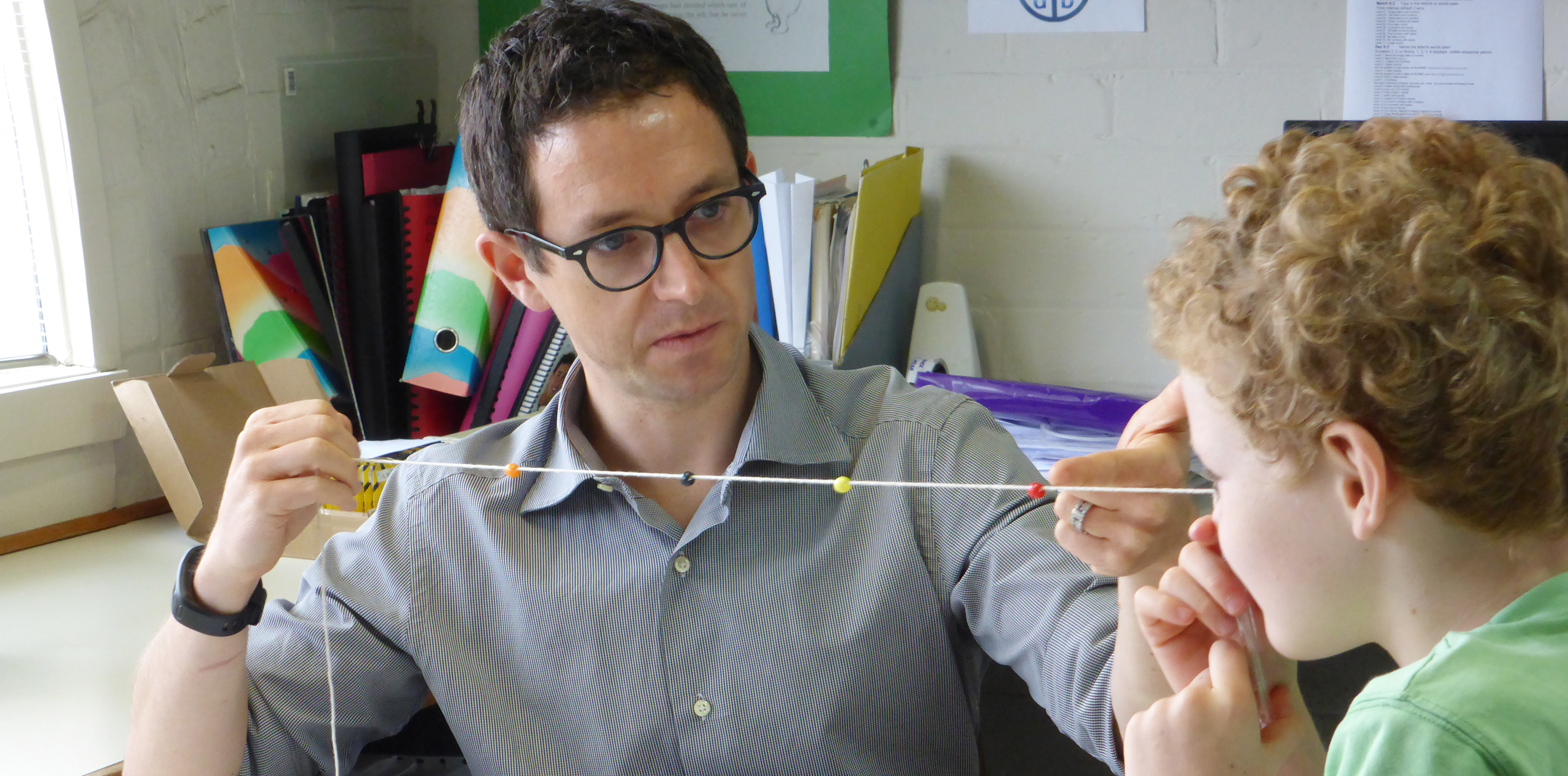
Peter Nixon with another of his patients (not Andrew)
______________________________
Behavioural optometrists Anne Pezzimenti and Peter Nixon present a vision therapy case study
Andrew was a smart and sporty nine-year-old when he first came in with his mother, Fiona.
Andrew said he loved sport and playing footy but wasn’t very good at it. He tended to miss marks and misjudge the ball, particularly when he had to look down to try to scoop up the ball.
His mother said that this really bothered Andrew, and he could become angry and tearful. She had tried to explain to Andrew that this was something he had to accept because of his eyes.
Fiona had a picture of Andrew at 12 months of age in which his eyes appeared straight. His eyes began to turn markedly and at the age of 15 months he was operated on to straighten his eyes. This was successful until Andrew was seven when his eyes began to turn again and he needed a second surgical procedure.
Fiona was devastated after the second surgical procedure when she was told that Andrew would not have depth perception and would not be able to catch a ball. This was a bitter pill to swallow for an increasingly sporty young boy.
Andrew’s frustration and his mother’s motivation led them to seek other options to improve his visual function.
Andrew had had a very good surgical outcome as cosmetically his eyes looked straight. His acuities were R 6/7 and L 6/6 and he did not have any significant refractive error. Closer inspection showed that Andrew struggled to use his right eye.
He showed dense right suppression with stereo testing and was unable to record any score with conventional stereopsis tests. He was able to obtain fleeting peripheral fusion with large Polaroid ring targets, but only when he stood slightly to one side.
He showed unstable use of his right eye, an intermittent small vertical deviation in some gaze positions, and difficulty converging this right eye when he tried to look up close—the type of distance that he would use to scoop up a football.
Andrew was advised that vision therapy may be an option and a preliminary trial of six vision therapy visits was suggested. Vision therapy initially targeted the development of strong monocular skills—accurate pursuits and saccade eye movements, spatial awareness with each eye, and normal control of dynamic eye focusing.
Andrew and his mother were very motivated. Fiona said that initially Andrew could look upwards with his right eye only for about three seconds. Following this, Andrew would become very uncomfortable and his eye would begin to tear. After vision therapy, this became effortless for Andrew and both eyes began to show the same ability.
Andrew worked with Peter Nixon and made rapid progress. By the fourth vision therapy visit, after about six weeks of activities, Andrew began to be able to ‘see’ with both eyes. He worked hard with activities that involved body movement and eye movement.
He particularly enjoyed being introduced to the iPad app called Vision Tap, which trained his ability to rapidly and consistently use both eyes together. With this program he began to be able to complete vergence activities, where he had to align targets rapidly and in all gaze positions.
When Andrew attended for the sixth review visit, he was bursting with pride. He had been selected for the school representative basketball team and he had recently won a sprint at school. Fiona explained that previously, running had been difficult for Andrew as his reduced spatial awareness had made him hesitant.
At review Andrew showed acuities of R 6/7+ and L 6/6. He achieved 120 seconds of arc (contour) stereopsis with the reindeer test (Wirt circles), and 100 seconds of stereopsis with shapes on the Randot Stereo Test. His vertical instability had disappeared. It was possible to perform normal binocular assessment now and measure fusional vergence ranges. He was able to successfully see physiological diplopia and align targets with the Brock string.
Because Andrew had made such rapid progress over the period of six vision therapy visits, with allied home activities, he was discharged at this point and left with some maintenance activities.
Fiona commented that after many surgeries, physiotherapy was used to re-establish best body function. She wondered why this was not used routinely with eyes. This is a good question. Behavioural optometry is best placed to fill this gap.