1:30min
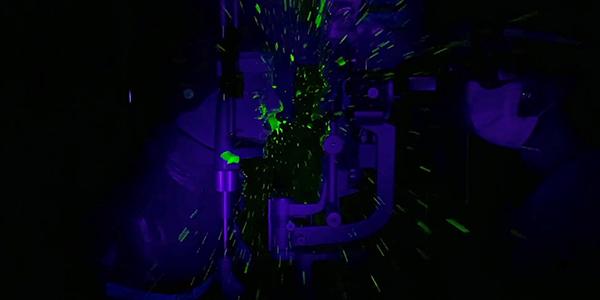
Simulated patient coughing showing droplet spread in JAMA Ophthalmology
By Helen Carter
Journalist
A video of a simulated patient having an eye examination shows that respiratory droplets can spread up to five metres after a patient coughs including onto the slitlamp, breath shield and the practitioner including their hair, hands, shoes and clothes.
The video highlights the importance of not only having a breath shield but of patients wearing masks in areas where coronavirus is endemic. It also highlights the importance of equipment disinfection and handwashing between patients and cleaning of rooms as the floor, walls and window coverings were also contaminated.
Standard personal protective equipment and breath shields did not eliminate the simulated spread of droplets, again emphasising the importance of masks, but researchers emphasised the importance of using breath shields or slitlamp barriers.
Canadian ophthalmologists Dr Tina Felfeli and Dr Efrem Mandelcorn released the video in June and published a research letter with findings of the simulated cough in JAMA Ophthalmology on August 18.
Flourescent dye enabled fluorescent respiratory droplets to be shown after the cough spreading through the air, falling onto equipment including the slitlamp, breath shield, practitioners’ arm, and clothes.
‘The greatest droplet spread was found on the slitlamp and the breath shield,’ they wrote.
‘Smaller droplet particles were noted up to five metres from the (patient) manikin.
‘This simulation suggests that the use of slitlamp breath shields and standard PPE does not eliminate the projection of droplets onto the examiner’s field and his or her chest, shoulders, and arms.
Droplets on practitioner’s hair, hands, shoes
‘The spread of smaller droplets was also identified on the hair, hands, and shoes of the examiner. Further contamination of the floor, walls, and window covers was identified within the room.
‘Findings support the use of adjuncts to the current standard PPE and protective barriers, such as breath shields to try to minimise cross contamination during slitlamp examinations.
‘Most importantly, the use of masks for the patient at the slitlamp should be further explored in future studies, because it may offer an easy and inexpensive means of providing protection for the examiner.’
Watch the simulated respiratory droplet spread during a slitlamp examination video.
The video illustrates simulation of a patient cough with spread of respiratory droplets during an ophthalmologic slitlamp examination. A cardiopulmonary resuscitation manikin was placed at the chin rest of a slitlamp and a latex balloon, compressed with oxygen and 1.25 mL of washable fluorescent dye, was run through tubing inside the oral cavity.
The balloon was inflated until it burst at 5 pounds per 72 square inches, which has been previously reported as the force for a voluntary cough and laryngeal cough reflex.
The simulation was performed under ultraviolet light conditions to visualise emission of small fluorescent particles and was repeated 10 times to confirm repeatability of results.
Australian simulation
A similar video evaluation by Australian doctors of a newly created Slit Lamp Shield made in Australia from plexiglass to reduce droplet exposure was published in Clinical and Experimental Optometry in May.
It found that without a shield, fluorescent dye was found on the clinician’s face shield, mask, gown, gloves, desk and the machine itself.
When the experiment was repeated with the shield in position, most of the dye was located on the outside of the shield, with smaller amounts on the clinicians’ gloves, desk and machine but there was no dye on the clinicians’ face shield or mask.
Preventing COVID-19 in 25 minutes
Optometrists, for an evidence based update on infection control during the COVID-19 pandemic covering how to protect you, your patients and staff, the best 25 minutes you can spend is watching this video from Optometry Australia’s Chief Clinical Officer, optometrist Luke Arundel.
Luke delivered this online presentation at Optometry Virtually Connected recently and refers to the Canadian video along with other research on PPE in his talk.
Also check out Optometry Australia’s online resources (COVID-19 optometry resources and update page for optometrists) which includes advice on “Should I be wearing a mask?”
Tagged as: COVID-19, Eye examinations, Patient management, Practice equipment